Kidney 101
Kidney Glossary
Renalus Center for Kidney Care believes in delivering accessible, educational content to our audience. Below you will find a glossary of kidney disease terms. To find a specific term, locate the alphabetical category for the keyword and click on the designated range (e.g. if you are looking for the definition of the word “albumin”, click “A-C”). Information posted below should NOT be a substitute for a visit to your doctor. Make sure to talk to a health professional if you have kidney problems.
-
A - C
Access – in dialysis, the point on the body where a needle or catheter is inserted. See arteriovenous fistula graft, vascular access, and catheter.
ACE Inhibitor – a medication that lowers blood pressure. ACE stands for angiotensin-converting enzyme. This medication also slows down kidney damage.
Acute – a condition that happens suddenly and is brief in appearance. This condition is the opposite of chronic conditions.
Acute Kidney Injury- a sudden and temporary loss of kidney function.
Acute Tubular Necrosis (ATN) – a severe form of acute kidney injury that develops when a person is a victim of a severe illness, infection, or has low blood pressure. Kidney function usually improves if the underlying disease is treated properly.
Antidiuretic Hormone (ADH) – a natural body chemical that slows down the body’s production of urine. Sometimes children lack normal amounts of this hormone leading to bed wetting.
Albumin – the major protein in blood. Large amounts of this protein in your urine may be a sign of chronic kidney disease. See urine albumin-to-creatinine ratio.
Albuminuria – a condition in which your urine has more than the normal amounts of albumin. This may be a sign of kidney disease.
Allograft – an organ or tissue transplant from one human to another.
Alport Syndrome – a genetic disorder that affects the cell membranes of your kidneys. It usually develops during early childhood. The condition can lead to end-stage renal disease. Symptoms are chronic blood and protein in urine.
Amino Acids – the basic building blocks of proteins.
Amyloidosis – a condition in which a protein-like material builds up in one or more organs. In kidneys, amyloidosis can lead to proteinuria, nephrotic syndrome, and kidney failure.
Analgesic-Associated Kidney Disease – loss of kidney function that results from long-term use of pain-relieving medications.
Anemia – a condition in which the number of red blood cells is lower than average. This results in less oxygen being carried to the body’s cells and can cause extreme fatigue.
Angiotensin – a substance in your blood that causes blood vessels to constrict, raising your blood pressure.
Antibiotic – a medication that kills bacteria.
Anuria – a condition in which your body stops making urine.
Angiotensin Receptor Blocker (ARB) – an oral medication that lowers your blood pressure.
Arteriovenous (AV) Fistula – surgical connection of an artery directly to a vein for people who will need hemodialysis. AV fistula causes the vein to grow thicker, allowing the repeated needle insertions required for hemodialysis. This is the primary method of vascular access. See hemodialysis under dialysis for more information.
Arteriovenous (AV) Graft – in hemodialysis, surgical connection of an artery to a vein using a soft, flexible tube, which can be used for repeated needle sticks. See hemodialysis under dialysis for more information.
Artery – a large blood vessel that carries blood with oxygen from the heart to all parts of the body.
Artificial Kidney – another name for a dialyzer.
Autoimmune Disease – a disorder in which the body’s immune system attacks and destroys body tissue instead of protecting the body from foreign substances, as it normally does. Examples are Goodpasture Syndrome and lupus erythematosus. See lupus nephritis.
Bacteria – tiny organisms that cause infection or disease.
Biopsy – a procedure in which a tiny piece of tissue, such as from the kidney or bladder, is removed for examination with a microscope.
Bladder – the balloon-shaped organ inside the pelvis that holds urine.
Blood Pressure – the force of blood exerted on the inside walls of blood vessels. Blood pressure is expressed as two numbers. For example, a blood pressure result of 120/80 is said as “120 over 80.” The first number is systolic pressure, or the pressure when the heart pushes blood out into the arteries. The second number is the diastolic pressure, or the pressure when the heart rests.
Blood Urea Nitrogen (BUN) – a waste product in the blood that comes from the breakdown of protein. The kidneys filter blood to remove urea. As kidney function decreases, the BUN level increases.
Bruit – a whooshing sound made when blood flows through a narrow vessel. A bruit in your abdomen may be a sign of renal artery stenosis.
Calcitriol – a hormone produced by the kidneys to help the body absorb dietary calcium into the blood and bones.
Calcium – a mineral the body needs for strong bones and teeth. Under certain conditions, calcium may form stones in the kidney.
Calcium Oxalate Stone – a kidney stone made from calcium and oxalate.
Catheter – a tube inserted through the skin into a blood vessel or cavity to draw out body fluid or infuse fluid. In peritoneal dialysis, a catheter is used to infuse dialysis solution into the abdominal cavity and drain it out again.
Chronic – refers to disorders that last a long time, often years. Chronic kidney disease may develop over many years and lead to end-stage renal disease. Chronic is the opposite of acute, or brief.
Chronic Kidney Disease (CKD) – any condition that causes reduced kidney function over a period of time. CKD is present when a patient’s glomerular filtration rate remains below 60 milliliters per minute for more than 3 months or when a patient’s urine albumin-to-creatinine ratio is over 30 milligrams of albumin for each gram of creatinine. CKD may develop over many years and lead to end-stage renal disease.
Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD) – abnormal bone hormone levels caused by the failure of the diseased kidneys to maintain the proper levels of calcium and phosphorus in the blood. CKD-MBD results in weak bones, a condition known as renal osteodystrophy. CKD-MBD is a common problem in people with kidney disease and affects almost all patients receiving dialysis.
Congenital Nephrotic Syndrome – a genetic kidney disease that develops before birth or in the first few months of life. Congenital nephrotic syndrome usually leads to end-stage renal disease and the need for dialysis or a kidney transplant by the second or third year of life.
Creatinine – a waste product from protein in the diet and from the normal breakdown of muscles in the body. Creatinine is removed from blood by the kidneys; as kidney disease progresses, the level of creatinine in the blood increases.
Creatinine Clearance – a test that measures how efficiently the kidneys remove creatinine from the blood. Low creatinine clearance indicates impaired kidney function.
Cross-Matching – before a transplant, the donor’s blood is tested with the recipient’s blood to see whether they are compatible.
Cyst – an abnormal sac containing gas, fluid, or a semisolid material. Cysts may form in the kidneys or in other parts of the body. See medullary sponge kidney, renal cysts, and polycystic kidney disease.
Cystine Stone – a rare form of kidney stone consisting of the amino acid cystine.
Cystinuria – a condition in which urine contains high levels of the amino acid cystine. If cystine does not dissolve in the urine, it can build up to form kidney stones.
Cystitis – inflammation of the bladder, causing pain and a burning feeling in the pelvis or urethra.
Cystoscope – a tubelike instrument used to look inside the urethra and bladder. The procedure is called cystoscopy.
-
D - F
Diabetes – a condition characterized by high blood glucose, resulting from the body’s inability to use blood glucose for energy. In type 1 diabetes, the pancreas no longer makes insulin, and therefore glucose cannot enter the cells to be used for energy. In type 2 diabetes, either the pancreas does not make enough insulin or the body is unable to use insulin correctly.
Diabetes Insipidus – a condition characterized by frequent and heavy urination, excessive thirst, and an overall feeling of weakness. This condition may be caused by a defect in the pituitary gland or the kidney. In diabetes insipidus, blood glucose levels are normal. See nephrogenic diabetes insipidus.
Dialysate – the part of a mixture that passes through a semipermeable membrane. The wastes from blood that pass into the dialysis solution become dialysate. The term dialysate is sometimes used as a synonym for dialysis solution.
Dialysis – the process of filtering wastes from the blood artificially. Filtering wastes is normally done by the kidneys. If the kidneys fail, the blood must be filtered artificially. The two major forms of dialysis are hemodialysis and peritoneal dialysis.
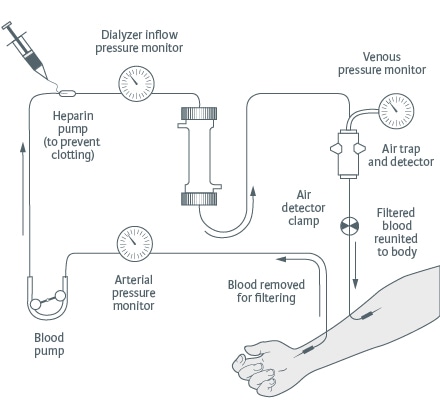
- Hemodialysis – the use of a machine to filter wastes from the blood after the kidneys have failed. The blood travels through tubes to a dialyzer, which removes wastes and extra fluid. The filtered blood then flows through another set of tubes back into the body.
- Peritoneal Dialysis – filtering the blood by using the lining of the abdominal cavity, or belly, as a semipermeable membrane. A cleansing liquid, called dialysis solution, is drained from a bag into the abdomen. Fluid and wastes flow through the lining of the abdominal cavity and remain “trapped” in the dialysis solution. The solution is then drained from the abdomen removing the extra fluid and wastes from the body. The two main types of peritoneal dialysis are continuous ambulatory peritoneal dialysis and continuous cycling peritoneal dialysis.
- Continuous Ambulatory Peritoneal Dialysis (CAPD) – a form of peritoneal dialysis that does not need a machine. With CAPD, the blood is always being filtered. The dialysis solution passes from a plastic bag through a catheter and into the abdomen. The dialysis solution stays in the abdomen. The dialysis solution stays in the abdomen with the catheter sealed. After several hours, the person using CAPD drains the solution back into a disposable bag. Then the person refills the abdomen with fresh solution through the same catheter to begin the filtering process again.
- Continuous Cycling Peritoneal Dialysis (CCPD) – a form of peritoneal dialysis that uses a machine. This machine automatically fills and drains the dialysis solution from the abdomen. A typical CCPD schedule involves three to five exchanges during the night while the person sleeps. During the day, the person using CCPD performs one exchange with a dwell time that lasts the entire day.
Dialysis Solution – a cleansing liquid used in the two major forms of dialysis — hemodialysis and peritoneal dialysis. Dialysis solution contains dextrose, a sugar, and other chemicals similar to those in the body. Dextrose draws wastes and extra fluid from the body into the dialysis solution. The term dialysate is sometimes used as a synonym for dialysis solution.
Dialyzer (pic) – an attachment to the hemodialysis machine. The dialyzer has two sections separated by a semipermeable membrane. One section holds dialysis solution. The other holds the patient’s blood. See hemodialysis under dialysis.
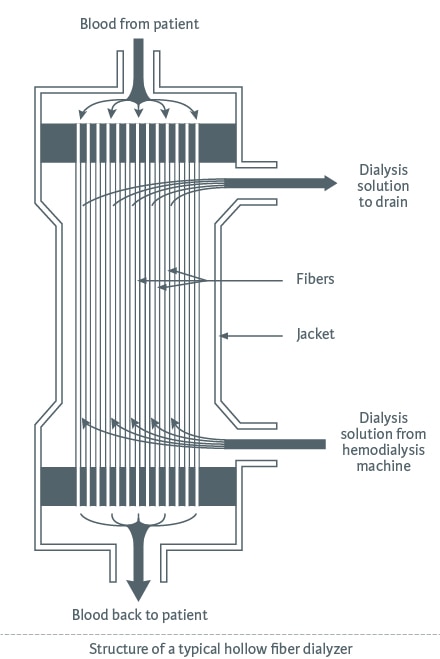
Diffusion – the tendency of molecules packed together in a small, dense area to spread out by crossing a semi-permeable membrane into a larger area with a lower concentration of molecules. In dialysis, wastes and excess electrolytes diffuse from blood to the dialysis solution.
Diuretic – an oral medicine that lowers blood pressure by aiding the kidneys removing fluid from the blood.
Donor – a person who gives blood, tissue, or an organ for transplantation. In kidney transplantation, the donor may be someone who is still alive, often a relative, or someone who just died. See transplant.
Dry Weight – the ideal weight for a person after a hemodialysis treatment. It is the weight at which a person’s blood pressure is normal and no swelling exists because all excess fluid has been removed. See hemodialysis under dialysis.
Dwell Time – in peritoneal dialysis the amount of time dialysis solution remains in the patient’s abdominal cavity between exchanges. See peritoneal dialysis under dialysis.
Edema – swelling caused by too much fluid in the body.
Electrolytes – chemicals in the body fluids and dialysis solution, including sodium, potassium, magnesium, and chloride. The kidneys control the amount of electrolytes in the body. When the kidneys fail, electrolytes get out of balance, causing potentially serious health problems. Dialysis can restore the balance.
End-Stage Renal Disease (ESRD) – total and permanent kidney failure. When the kidneys fail, the body retains fluid. Harmful wastes build up. A person with ESRD needs treatment to replace the work of the failed kidneys.
Erythropoietin – a hormone made by the kidneys to help form red blood cells. Lack of this hormone may lead to anemia.
Exchange – in peritoneal dialysis, the draining of used dialysis solution from the abdomen, followed by refilling with a fresh bag of solution. See peritoneal dialysis under dialysis.
Extracorporeal Shock Wave Lithotripsy – a nonsurgical procedure using shock waves to break up kidney stones.
Feces – the solid waste that passes through the rectum as a bowel movement. Feces are undigested food, bacteria, mucus, and dead cells.
- Hemodialysis – the use of a machine to filter wastes from the blood after the kidneys have failed. The blood travels through tubes to a dialyzer, which removes wastes and extra fluid. The filtered blood then flows through another set of tubes back into the body.
-
G - I
Glomerular Filtration Rate (GFR) – the rate at which the kidneys filter wastes and extra fluid from the blood, measured in milliliters per minute.
Glomeruli – plural of glomerulus.
Glomerulonephritis – inflammation of the glomeruli. Most often, it is caused by an autoimmune disease, but it can also result from infection.
Glomerulosclerosis – scarring of the glomeruli. It may result from diabetes or from deposits in parts of the glomeruli (focal segmental glomerulosclerosis). The most common signs of glomerulosclerosis are proteinuria and chronic kidney disease.
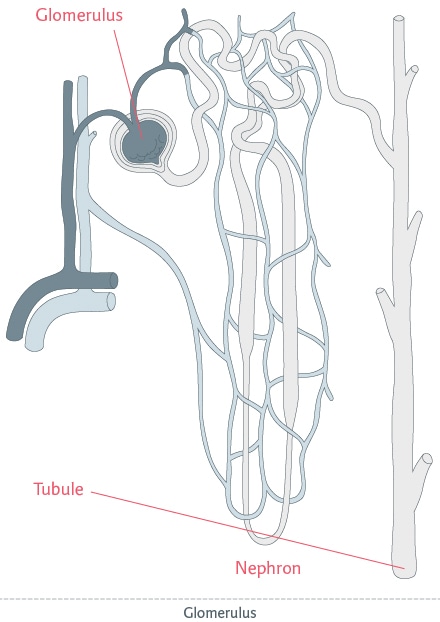
Glomerulus – a tiny set of looping blood vessels in the nephron where blood is filtered in the kidney.
Goodpasture Syndrome – a rare disease that usually includes bleeding from the lungs, coughing up blood, and inflammation of the kidneys that can lead to kidney failure. This condition is an autoimmune disease.
Graft – in a transplant, the transplanted organ or tissue. See also arteriovenous graft.
Hematocrit – a measure that tells what portion of a blood sample consists of red blood cells. Low hematocrit suggests anemia or massive blood loss.
Hematuria – blood in the urine, which can be a sign of a kidney stone, glomerulonephritis, or other kidney problem.
Hemolytic Uremic Syndrome (HUS) – a disease that affects the blood and blood vessels. It destroys red blood cells, cells that cause the blood to clot, and the lining of the blood vessels. HUS is often caused by the Escherichia coli bacterium in contaminated food. People with HUS may develop acute kidney injury.
Henoch- Schönlein Purpura (HSP) – an autoimmune disease affecting mostly children between ages 2 and 11 that causes the blood vessels in the skin to swell. Rashes and bruising are the main symptoms. Kidney damage results in a small percentage of children with HSP.
Hormone – a natural chemical produced in an organ or gland and released into the blood to trigger or regulate particular body functions. The kidney releases three hormones: erythropoietin, renin, and calcitriol.
Hydronephrosis – swelling of the kidney and renal pelvis, usually because something is blocking urine from flowing into or out of the bladder.
Hydroureter – swelling of the ureter, usually because something is blocking urine from flowing into or out of the bladder.
Hypercalciuria – abnormally large amounts of calcium in the urine.
Hyperkalemia – abnormally large amounts of potassium in the blood, often as a result of poor kidney function or inadequate dialysis.
Hyperoxaluria – unusually large amounts of oxalate in the urine, leading to kidney stones.
Hypertension – a condition present when blood flows through the blood vessels with a force greater than normal. Also called high blood pressure. Hypertension can strain the heart, damage blood vessels and increase the risk of kidney problems, heart attack, stroke and death.
Hypokalemia – abnormally small amounts of potassium in the blood, often as the result of a kidney defect, including some forms of renal tubular acidosis.
IgA Nephropathy – a kidney disorder caused by deposits of the protein immunoglobulin A (IgA) inside the glomeruli (filters) within the kidney. The IgA protein damages the glomeruli, leading to blood and protein in the urine, swelling in the hands and feet, and sometimes kidney failure.
Immune System – the body’s system for protecting itself from viruses and bacteria or any foreign substances.
Immunosuppressant – a drug given to stop the natural responses of the body’s immune system. Immunosuppressants are given to prevent organ rejection in people who have received a transplant and to people with certain autoimmune diseases, like lupus.
Inflammation – swelling and redness that results from injury to tissue.
Insulin – a hormone that helps the body use glucose for energy. The beta cells of the pancreas make insulin. When the body cannot make enough insulin, insulin must be taken by injection or other means.
Interstitial Nephritis – inflammation of the kidney cells that are not part of the fluid-collecting units. Interstitial nephritis is a condition that can lead to acute kidney injury or chronic kidney disease.
Intravenous Pyelogram – an x-ray of the urinary tract. A dye is injected into a vein in the patient’s arm to make the kidneys, ureters, and bladder visible on the x-ray and to show any blockage in the urinary tract.
-
J - N
Kidney – one of the two bean-shaped organs that filter wastes from the blood. The kidneys are located near the middle of the back, one on each side of the spine. They create urine, which is delivered to the bladder through tubes called ureters.
Kidney Dysplasia – a condition in which the internal structures of one or both of a baby’s kidneys do not develop normally while the baby is growing in the womb. Fluid-filled sacs called cysts replace normal kidney tissue. Kidney dysplasia usually happens in only one kidney.
Kidney Failure – loss of kidney function.
Kidney Function – the amount of work done by the kidneys. A decline in kidney function means the kidneys are not filtering wastes and fluid from the blood as well as they should.
Kidney Stone – a stone that develops from crystals that form in urine and build up on the inner surfaces of the kidney, in the renal pelvis, or in the ureters. Kidney stones include calcium oxalate stones, cystine stones, struvite stones and uric acid stones.
Kt/V – a measurement of dialysis dose. The measurement takes into account the efficiency of the creatinine clearance, the treatment time, and the total volume of urea in the body. Kt/V is also used in determining the adequacy of peritoneal dialysis.
Lithotripsy – a method of breaking up kidney stones by using shock waves or other means.
Lupus Nephritis – inflammation of the kidneys caused by an autoimmune disease called systemic lupus erythematosus. The condition can cause hematuria and proteinuria, and it may progress to end-stage renal disease.
Medullary Sponge Kidney – a birth defect in which cysts form in the central part of the kidney, causing a spongelike appearance and blocking the flow of urine through the tubules.
Membranoproliferative Glomerulonephritis (MPGN) – a disease in which inflammation leads to scarring in the glomeruli, causing proteinuria, hematuria, and sometimes chronic kidney disease or end-stage renal disease. MPGN occurs primarily in children and young adults.
Membranous Nephropathy – a disorder that hinders the kidneys’ ability to filter wastes from the blood because of harmful deposits on the glomerular membrane. Some cases of membranous nephropathy develop after an autoimmune disease or malignancy, but most develop without a known cause.
Nephrectomy – surgical removal of a kidney.
Nephrogenic Diabetes Insipidus – constant thirst and frequent urination because the kidney tubules cannot respond to antidiuretic hormone. The result is an increase in urine formation and excessive urine flow.
Nephrolotihiasis – the condition of having kidney stones.
Nephrologist – a doctor who treats people who have kidney problems or related conditions, such as hypertension.
Nephrology – a branch of medicine concerned with diseases of the kidneys.
Nephron – a tiny part of the kidneys. Each kidney is made up of about 1 million nephrons, which are the working units of the kidneys, removing wastes and extra fluids from the blood.
Nephropathy – disease of the kidneys.
Nephrostomy – a catheter, or tube, inserted into the kidney through the skin to allow urine to drain directly through the skin, allowing urine to drain directly from the kidney into an external bag.
Nephrotic Syndrome – a collection of symptoms that indicate kidney damage. Symptoms include high levels of protein in the urine, lack of protein in the blood and high blood cholesterol.
Nuclear Scan – a test of the structure, blood flow and function of the kidneys. The doctor injects a mildly radioactive solution into a patient’s arm vein and uses x-rays to monitor its progress through the kidneys.
-
O - R
Osmosis – movement of water across semipermeable membrane from a diluted area to a more concentrated area.
Oxalate – a chemical that combines with calcium in urine to form the most common type of kidney stone, the calcium oxalate stone.
Pancreas – an organ that makes insulin and enzymes for digestion. The pancreas is located behind the lower part of the stomach and is about the size of a hand.
Pelvis – the bowl-shaped bone that supports the spine and holds up the digestive, urinary and reproductive organs. The legs connect to the body at the pelvis.
Percutaneous Nephrolithotomy – a method for removing kidney stones via surgery through a small incision in the back.
Peritoneal Cavity – the space inside the lower abdomen, but outside the internal organs.
Peritoneum – the semipermeable membrane lining the peritoneal cavity.
Peritonitis – inflammation of the peritoneum, a complication of peritoneal dialysis.
Phosphate – phosphorus combined with oxygen.
Phosphate Binders – medications that bind phosphate in the digestive tract so that phosphate leaves the body as feces.
Phosphorus – a mineral found in many foods, such as beans, nuts, milk and meat. Too much phosphorus in the blood pulls calcium from the bones.
Pituitary Gland – a pea-sized gland at the base of the brain that regulates the body’s balance of hormones.
Polycystic Kidney Disease (PKD) – an inherited disorder characterized by many grapelike clusters of fluid-filled cysts that make both kidneys larger over time. These cysts take over and destroy working kidney tissue. PKD may cause chronic kidney disease and end-stage renal disease.
Potassium – a mineral and electrolyte found in the body and in many foods.
Protein – 1. One of the three main nutrients in food. Foods that provide protein include meat, poultry, fish, cheese, milk, dairy products, eggs and dried beans. 2. Proteins are also used in the body for cell structure, fighting infection and other functions. After the body’s cells use protein, it is broken down into waste products containing nitrogen that must be removed by the kidneys. The blood absorbs amino acids and uses them to build and mend cells.
Proteinuria – a condition in which the urine contains large amounts of protein, a sign that the kidneys are damaged.
Pyelonephritis – an infection of the kidneys, usually caused by a germ that has traveled up through the urethra, bladder, and ureters from outside the body.
Renal – of or relating to the kidneys. A renal disease is a disease of the kidneys. Renal failure means the kidneys are damaged.
Renal Agenesis – the absence or severe malformation of one or both kidneys.
Renal Artery Stenosis – narrowing of the artery that supplies blood to the kidney often resulting in hypertension and kidney damage.
Renal Cell Carcinoma – a type of kidney cancer.
Renal Cysts – abnormal fluid-filled sacs in the kidney that range from microscopic to much larger. Many simple cysts are harmless, while other types can seriously damage the kidneys.
Renal Osteodystrophy – weak bones caused by chronic kidney disease-mineral and bone disorder. Renal osteodystrophy is a common problem for people on dialysis who have high phosphate levels or insufficient vitamin D supplementation.
Renal Pelvis – the basin into which the urine formed by the kidneys is excreted before it travels to the ureters and bladder.
Renal Tubular Acidosis – a defect in the kidneys that hinders their normal excretion of acids. Failure to excrete acids can lead to weak bones, kidney stones and poor growth in children.
Renal Vein Thrombosis – blood clots in the vessel that carries blood away from one of the kidneys. This condition can occur in people with nephrotic syndrome.
Renin – a hormone made by the kidneys that helps regulate the volume of fluid in the body and blood pressure.
-
S - U
Semipermeable Membrane – a thin sheet, or layer, of tissue that lines a body cavity or separates two parts of the body. A semipermeable membrane can act as a filter, allowing some particles to pass from one part of the body to another while keeping other particles in place. In hemodialysis, the artificial membrane in a dialyzer acts as the semipermeable membrane filtering waste products from the blood. In peritoneal dialysis, the peritoneum acts as the semipermeable membrane.
Sodium – a mineral and electrolyte found in the body and in many foods.
Struvite Stone – a type of kidney stone caused by infection.
Thrill – a vibration or buzz that can be felt in an arteriovenous fistula, an indication that blood is flowing through the fistula.
Transplant – placement of a healthy organ into the body to take over the work of a damaged organ. A kidney transplant may come from a living donor, often a relative, or from someone who has just died.
Tubule – one of millions of tiny structures within the kidneys that collect urine from the glomeruli.
Ultrafiltration (UF) – in dialysis the process by which fluid from the blood passes through a semipermeable membrane into a dialysis solution. In peritoneal dialysis, UF is measured as the volume of solution drained at the end of an exchange minus the volume of solution filled at the beginning of the exchange.
Ultrasound – a technique that bounces safe, painless sound waves off organs to create an image of their structure.
Urea – a waste product found in the blood that results from the normal breakdown of protein in the liver. Urea is normally removed from the blood by the kidneys and then excreted in the urine. Urea accumulates in the body of people with kidney failure.
Urea Reduction Ratio (URR) – a blood test that compares the amount of blood urea nitrogen before and after dialysis to measure the effectiveness of the dialysis dose.
Uremia – the illness associated with the buildup of urea in the blood because the kidneys are damaged. Symptoms include nausea, vomiting, loss of appetite, weakness and mental confusion.
Ureteroscope – a tool for examining the bladder and ureters and for removing kidney stones through the urethra. The procedure is called ureteroscopy.
Ureters – tubes that carry urine from the kidneys to the bladder.
Urethra – the tube that carries urine from the bladder to the outside of the body.
Uric Acid Stone – a kidney stone that may result from a diet high in animal protein. When the body breaks down this protein, uric acid levels rise and can form stones.
Urinalysis – a test of a urine sample that can reveal many problems of the urinary tract and other body systems. The sample may be observed for color, cloudiness, and concentration; signs of drug use; chemical composition, including glucose; the presence of protein, blood cells, or germs; or other signs of disease.
Urinary Tract – the system that takes wastes from the blood and carries them out of the body in the form of urine. The urinary tract includes the kidneys, renal pelvises, ureters, bladder, and urethra.
Urinary Tract Infection (UTI) – an illness caused by harmful bacteria growing in the urinary tract.
Urinate – to release urine from the bladder to the outside of the body.
Urine – liquid waste product filtered from the blood by the kidneys, stored in the bladder, and expelled from the body through the urethra by the act of voiding, or urinating. See urinate and void.
Urine Albumin-to-Creatinine Ratio (UACR) – a measurement that compares the amount of albumin with the amount of creatinine in a urine sample. A patient has chronic kidney disease if the UACR is over 30 milligrams (mg) of albumin for each gram (g) of creatinine (30 mg/g).
Urolithiasis – the condition of having stones in the urinary tract.
-
V - Z
Vascular Access – a general term to describe where blood is removed from and returned to the body during hemodialysis. A vascular access may be an arteriovenous fistula, an arteriovenous graft, or a catheter. See hemodialysis under dialysis.
Vasculitis – inflammation of the blood vessel walls. This swelling can cause rashes and diseases in multiple organs of the body, including the kidneys.
Vein – a blood vessel that carries blood to the heart.
Venous Line – in hemodialysis, tubing that carries blood from the dialyzer back to the body. See hemodialysis under dialysis.
Vesicoureteral Reflux – an abnormal condition in which urine backs up into the ureters, and occasionally into the kidneys, raising the risk of infection.
Void – to urinate; to empty the bladder.
Wegener’s Granulomatosis – an autoimmune disease that damages the blood vessels and causes disease in the lungs, upper respiratory tract and kidneys.

